In this guest post, Chris Deed from The Pure Food Co discusses a recent food and nutrition trial they did with Uniting NSW.ACT (Sydney Central), which has shown positive results in addressing weight loss. This program has been shortlisted in this year’s Future of Ageing Awards.
There are many myths surrounding ageing, particularly when it comes to food and nutrition. Some people may believe that malnutrition, unplanned weight loss and a reduced appetite are simply part of getting older, but this doesn’t have to be the case, in fact food can and should play a significant role in supporting healthy ageing.
We recently partnered with Uniting NSW.ACT (Sydney Central) for a six-week pilot study to address the nutritional needs of its residents experiencing weight loss from reduced appetite and challenges with eating due to issues such as dysphagia. We believed if we got the food and nutrition right, many of these risks would be reduced.
The clinical outcomes demonstrated how modified textured meals and protein-rich smoothies can effectively address both weight loss and weight gain. By targeting the specific nutritional requirements for the group of Uniting NSW.ACT (Sydney Central) residents, the trial highlighted the importance of prioritising protein in modified textured diets of aged care residents to support their weight gain.
The study involved two groups of aged care residents receiving texture-modified meals and smoothies across four Uniting NSW.ACT (Sydney Central) sites with two different nutrition programs.
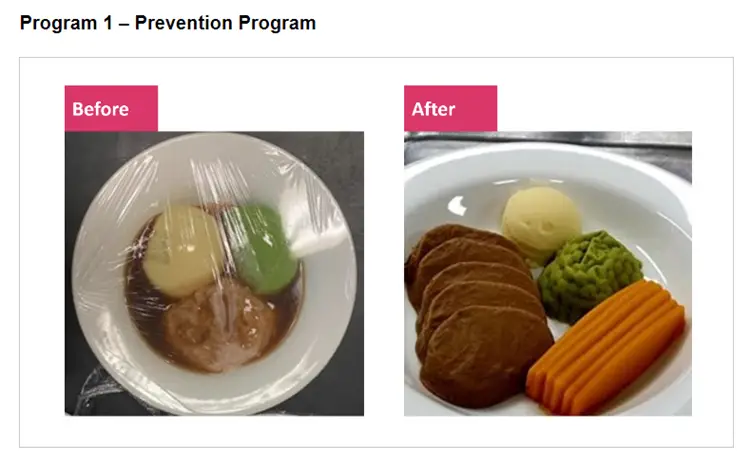
The prevention strategy targeted residents at higher risk of malnutrition and weight loss. Over six weeks, 30 residents were served nutritious texture-modified meals.
Before the study, over half (55%) of the residents had lost weight but within four weeks of being on the program, nearly three-quarters (72%) had gained weight.
In the targeted intervention trial, 43 residents experiencing unplanned weight loss received high– energy, high-protein smoothies twice a day during mid meals, significantly boosting their protein, energy and calcium intake.
Before the study, all residents had been losing weight, with 75% continuing to lose weight in the month before the program’s launch. Following the smoothie trial, more than half (54%) of residents either maintained or gained weight, with 11 residents gaining over one kilogram. *(The trial faced a setback at one site due to COVID-19, disrupting smoothie deliveries).
The results highlight the impact of nutritional intervention to address unplanned weight loss, and by also focusing on taste and presentation, residents have the opportunity to once again enjoy the entire experience of eating.
This study also demonstrates the intrinsic link between protein and wound healing. Both programs monitored pressure injuries to assess the impact of increased protein on wound healing. The results were resounding, showing that 100% of wounds healed due to enhanced protein absorption from the trial.
The emphasis on protein in the study underscores its importance not only in combating weight loss but also in promoting weight gain in elderly residents in aged care settings. By ensuring correct protein intake through the tailored intervention program, residents gained weight, their wounds healed and their sense of well-being improved.
During the trial with Uniting NSW.ACT (Sydney Central), clinical teams received training on the importance of nutrition tailored to the needs of the residents and they were educated on the key benefits of the textured modified meals and how these products can make the dining experience less confronting and more enjoyable.
Additionally, extensive training sessions were conducted with the kitchen team to streamline operational processes. Following the trials, Uniting NSW.ACT (Sydney Central) implemented a textured modified meal delivery across 35 of its sites.
By 2050, more than 3.5 million Australians are expected to access aged care services. This will increase the demand for texture-modified foods, which are complex to prepare, putting more pressure on aged care providers, clinical teams and kitchens. Often staff rely on their food knowledge and training, but many residents need nutritional food for medical reasons, and as the population ages, that may not be enough.