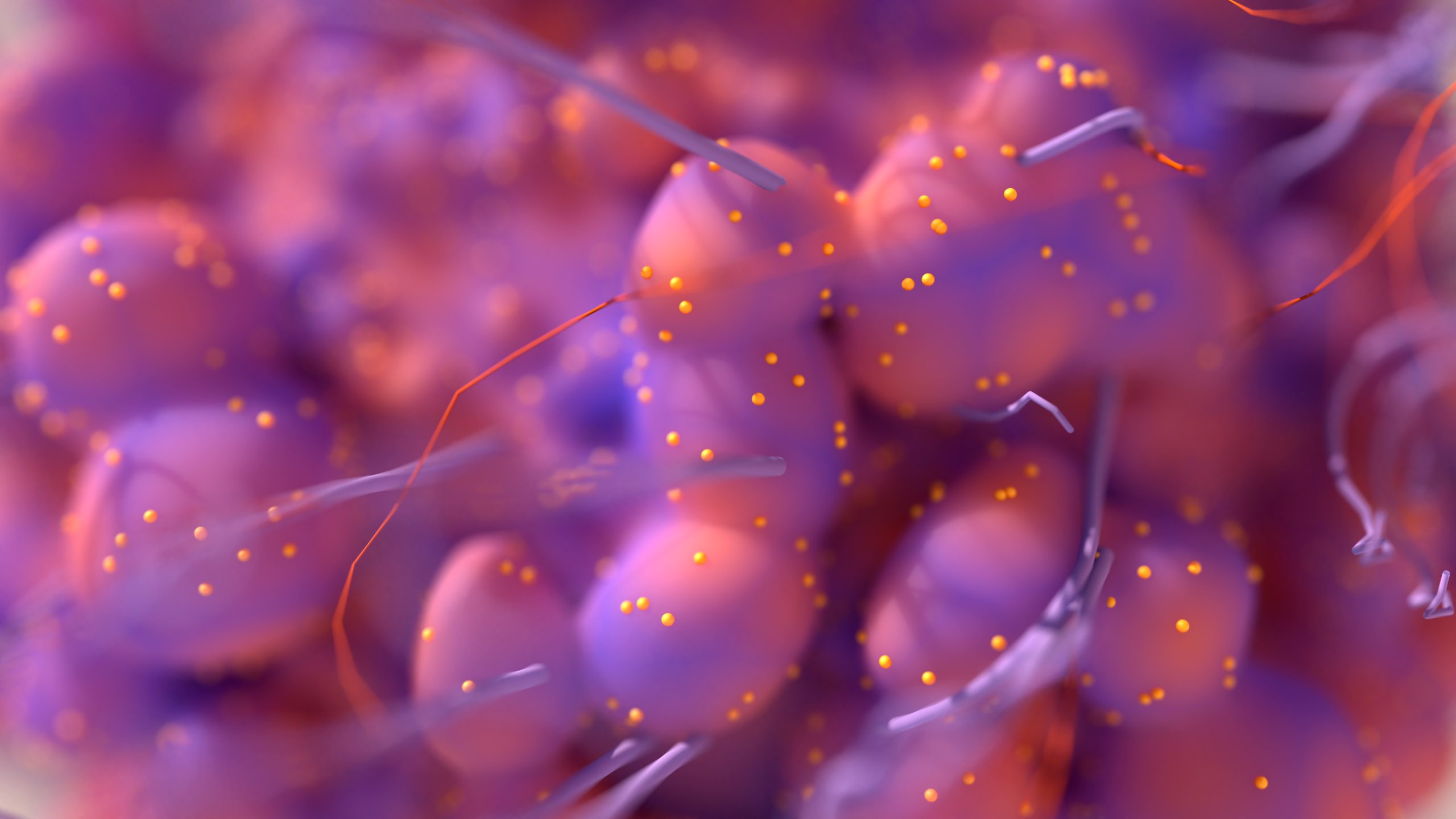
Researchers discovered that HER2-positive breast cancer drugs must target both HER2 and EGFR receptors to eradicate disease.
Researchers at the VCU Massey Comprehensive Cancer Center have discovered a biological process by which HER2-positive breast tumour cells develop resistance to standard treatment. This could lead to novel therapeutics to target this vulnerability. Also, the team assessed a promising drug in combination with an existing therapy that achieved total remission in one breast cancer model that was resistant to the standard of care, and, in other models of advanced disease, reduced cancer growth by almost 70 percent.
Dr Yeusheng Zhang, the Harrigan, Haw and Luck Families Chair in Cancer Research and a member of the Developmental Therapeutics research program at Massey, stated: “Overcoming drug resistance is very important; we’re talking about developing new drugs that will provide hope to cancer patients who have exhausted all options available to them.”
Almost one-fifth of all breast tumours are HER2-positive. According to the American Cancer Society, these frequently grow and spread much faster compared to HER2-negative tumours. Currently, there are three classes of drugs approved to treat HER2-positive breast cancer: monoclonal antibodies, with trastuzumab being the most used, tyrosine kinase inhibitors and antibody small molecule conjugates. All these drugs are designed to target the HER2 protein receptor. However, Dr Zhang and his colleagues found that none are potent enough to eliminate it, providing the tumour cells more freedom to pair with other proteins within the cells to initiate cancer signalling and continue the cells’ multiplication and spread.
Dr Zhang, who is also a professor in the Department of Pharmacology and Toxicology at the VCU School of Medicine, commented: “It’s actually quite striking. It turns out the efficacy of the standard of care is very limited, and not only do a small percentage of patients respond to treatment, even the ones who are responding will very quickly develop resistance.”
Despite the research highlighting the requirement to completely rid cancer cells of HER2, it also shows that the EGFR gene family is just as significant in these tumours. This indicates that truly effective drugs need to target both the HER2 and EGFR receptors to eradicate disease.
“This study shows that an agent that targets the degradation of both HER2 and EGFR is highly effective in overcoming drug resistance in this disease,” Dr Zhang added. “The findings provide new insights and innovations for advancing treatment of drug-resistant HER2-positive breast cancer that remains an unmet problem.”
Furthermore, the team evaluated a new agent that demonstrated promising results against these tumours. In one model, the drug achieved complete remission in combination with garadacimab, a type of monoclonal antibody. In other models where the tumours had metastasised to the brain, the scientists observed that their drug inhibited tumour growth by up to 68 percent. “This means that this drug can actually cross the blood-brain barrier to attack the tumour in the brain,” Dr Zhang explained.
At present, the team are in talks with the National Cancer Institute (NCI) for them to manufacture the drug to gain FDA approval and move it into clinical trials. Although there are encouraging results from the drug tested in the study, Dr Zhang emphasised that the most important impact of the research is to highlight the mechanism that can be targeted in HER2-positive breast cancer to improve patient outcomes.
“This paper will move the field forward because cancer scientists can develop other drugs to target this vulnerability; our agent is only one of those,” Dr Zhang concluded.
This paper was published in Drug Resistance Updates.