New research led by the Doherty Institute sheds light on the complex behaviour of key immune cells, known as CD4+ T cells, in the spleen in response to a malaria infection thanks to cutting-edge technology.
CD4+ T cells, often referred to as “helper T cells”, are integral in the defence against malaria-causing parasites. They transform into various types of cells to help clear the infection primarily specialising in either infection-fighting roles or aiding in antibody production. Although previous studies hinted at the diversity and complexity of these immune cells during infection, their actual behaviour and interactions with other cells have remained unknown.
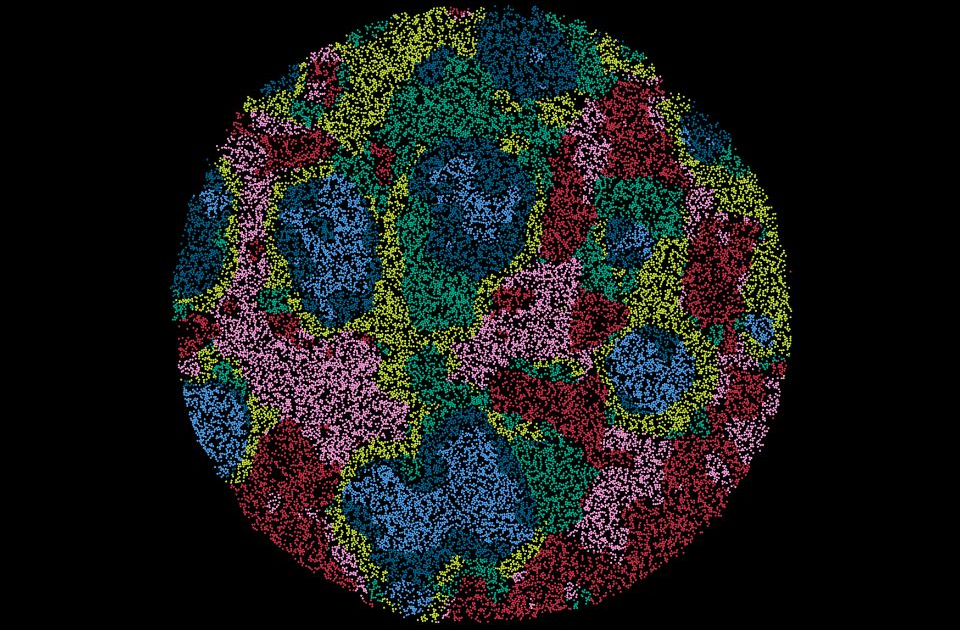
A team of researchers, led by University of Melbourne’s Associate Professor Ashraful Haque, Lab Head at the Doherty Institute, employed advanced technology called spatial transcriptomics, also known as tissue genomics, to create detailed maps of spleen tissue during malaria infection. This technique allowed them to see where different types of cells are located and how they interact, providing valuable insights into their roles and mechanisms.
They observed that the infection-fighting cells tend to gather in specific areas of the spleen, close to other immune cells where they work together to mount an effective immune response against the malaria parasite.
They also discovered the importance of a specific gene which can control the growth and function of the helper T cells.
While the researchers tested this method on the immunity in malaria using spleen tissue, it can be applied to various fields, such as developmental biology, cancer, immunology and neuroscience.
University of Melbourne’s Cameron Williams, a final year PhD student at the Doherty Institute and lead author of the study said this research, published in Cell Reports, is among the first to illustrate how this technology can be used to study complex cell processes.
“We are entering a new era of cellular exploration. This is a technology that everyone is clamouring for as it allows scientists to observe cellular interactions and listen in on the hidden conversations between cells,” said Dr Williams.
This study adds to the body of knowledge on the Human Cell Atlas project, a global consortium mapping approximately 37 trillion cells in the human body. The project is expected to significantly improve the diagnosis and treatment of various illnesses.
Associate Professor Haque emphasised the potential of tissue genomics for studying biological processes and diseases.
“Previously, when we interrogated cells to find out more about them, it was like interviewing them in a quiet room away from any stimuli. Our new approach is like observing them in a bustling street, where we can see their work and behaviours in the dynamic environment of the actual tissue they are in,” said Associate Professor Haque.
“As this technology continues to advance, it promises to transform medical research and treatment in areas such as cancer biology, developmental processes and tissue regeneration. By understanding how cells interact and communicate in their native environment, we can identify new therapeutic targets and develop more effective treatments.”
Spatial transcriptomics marks a significant leap forward in our understanding of the complex behaviour of immune cells by providing unprecedented level of detail in cellular mapping. It has the potential to transform our approach to studying diseases like malaria and inform the development of new vaccines and treatments.