In a busy hospital waiting room, a young man’s muscles began contracting in a harsh, unyielding spasm as a quick-acting student rushed to his aid.
“We ran over to help stabilize the patient. To my surprise, his mother calmly reassured us that his seizure was a routine occurrence due to his epilepsy,” said Seth Lieberman, Ph.D. ’21, D.V.M. ’24, who was an undergraduate student at the time.
Lieberman would later witness a second seizure – ironically involving a professor giving a lecture on epilepsy – and many canine seizures while working in the Cornell University Hospital for Animals as a graduate student in the College of Veterinary Medicine. These experiences led him to learn more about the disease and ignited a passion to help those who suffer from it.
Today, Lieberman is part of an interdisciplinary Cornell research team that has developed a new surgical technique that blocks the spread of focal epileptic seizures in the brain by making precise incisions with femtosecond laser pulses. The promising new approach, detailed in the journal Advanced Science, offers several advantages to existing treatment protocols.
Limited treatment options
Epilepsy, characterized by chronic seizures due to uncontrolled excitatory brain activity, affects approximately one in 26 people over their lifetime and is also the most common neurologic disorder in dogs.
Focal epilepsy, a subclass of the disease, involves seizures originating from a localized brain region before spreading to surrounding tissue. While medications can manage epilepsy in many cases, about 45% of focal epilepsy patients are resistant or become resistant over time. For those individuals, treatment often involves surgical removal of the epileptic part of the brain.
“The issue is when you remove a large area of brain; sometimes that part is functional,” said Dr. Theodore Schwartz, the David and Ursel Barnes Professor of Minimally Invasive Neurosurgery at Weill Cornell Medicine, who co-authored the study.
An alternative that has emerged in recent years, laser interstitial thermal therapy, uses a laser to heat up the targeted brain region, effectively killing the source of the seizures but also killing any normal function associated with that region.
“It’s only really useful if you have a deep area of the brain that’s not greater than about 2 or 3 centimeters in size,” Schwartz said.
Removing or burning an epileptic region of the brain comes with the risks of blindness, nerve loss, chronic pain, stroke and memory loss, among many other neurologic deficits, which is why Schwartz began doing research on a new solution – one that was inspired by an unavailing surgical method established more than 50 years ago.
Modernizing a ‘barbaric’ procedure
Twentieth-century advances in understanding epilepsy revealed that focal seizures typically initiate in one part of the brain’s gray matter and propagate to adjacent brain regions in specific layers, perpendicular to connections important for normal brain function. This knowledge led to the development of multiple subpial transections, a surgical method first published in 1973, which aims to prevent seizure spread by making small incisions in the cortex, effectively cutting off the seizure’s route through the brain. However, the technique saw limited clinical adoption.
“It was a very barbaric operation where you basically take a bent wire and scrape it through the brain,” Schwartz said. “It caused a lot of trauma to the brain and it was an uncontrolled, blind operation.”
But the concept behind the surgery – cutting off the seizure’s spread while leaving as much of the brain intact as possible – had its merits. Schwartz’s idea was to modernize the procedure by replacing the wire with a more precise and guided tool. After investigating the idea preliminary as a neurosurgery resident, Schwartz then turned to Chris Schaffer, professor of biomedical engineering and co-author of the study, who develops ultra-precise laser scalpels and imaging techniques in his lab. The two met at a Cornell conference and began discussing how they could work together.
“We had this idea that if we could build the right scalpel, we could reinvigorate this idea from the 1970s and maybe build it in a way where it could translate across the neurosurgical community,” Schaffer said. “That is what launched us into trying to use this femtosecond laser scalpel.”
Engineering and testing a laser scalpel
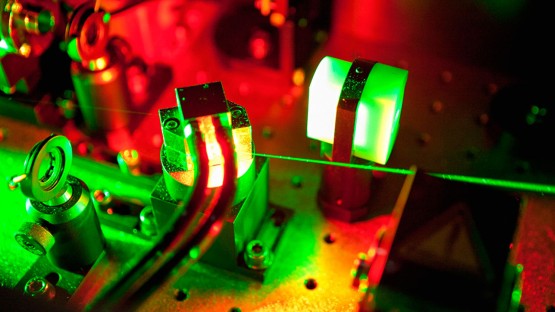
Schaffer’s lab uses tightly focused, femtosecond-duration, infrared laser pulses to produce cuts inside a biological sample without affecting overlying tissue. A femtosecond is one-quadrillionth of a second. This technique is crucial for targeting the right cortical layer to halt seizures while preserving the blood vessels on the brain’s surface.
The system was optimized to produce cuts about 55 microns thick that could be placed up to 1 millimeter into the brain, the depth needed to treat non-human subjects for the study.
When it came time to test the laser, Schaffer recruited one of his doctoral students at the time, Lieberman, who coincidentally had met Schwartz when the surgeon spoke at Lieberman’s high school in Connecticut several years prior.
“Dr. Schwartz inspired my initial interest in neuroscience and neurosurgery during that high school lecture,” Lieberman said. “When I discovered he was the neurosurgeon collaborator for this project, the full-circle moment reinforced my commitment.”
The laser scalpel was used to perform surgeries on mice with epilepsy, which were then monitored for 3 to 12 months. The results were “incredibly promising,” according to Lieberman. The procedure reduced seizure frequency in most subjects by 87%. For the few seizures that still occurred, 95% of them were blocked from spreading to the rest of the brain.
Regarding the risks of the procedure, the surgery caused a modest, transient decrease in cortical blood flow. However, when applied to the brain area controlling movement, the laser cuts did not result in significant deficits in the subjects’ motor task performance, indicating the procedure did not notably impact brain structure or function.
“The results were better than we had hoped,” Schwartz said. “If one were interested in creating a treatment for epilepsy using these principles, I think we’ve shown this would be a very effective method.”
Eye on the OR
One remaining question is how to translate the approach into the operating room, where the laser will have to reach into much larger and more complex brains, such as those of dogs and humans. The researchers hope to pursue an upgrade to the laser scalpel that would increase light penetration to greater depths, traverse folds in the brain without damaging surrounding tissue, and better pinpoint the seizure focus.
“It would need a feedback mechanism that could look at the brain, see where the surface blood vessels are, and make its cuts robotically without damaging them,” Schwartz said. “It wouldn’t be easy to do, but all of those are technical engineering issues that can potentially be overcome.”
Lieberman envisions the most immediate application for veterinary medicine, and said reducing the seizure frequency in dogs by even 50% would be considered a successful outcome. Ultimately, providing treatment for canines and humans is his goal.
“The excitement I felt when I first saw a seizure localized to just the focus area in our study was indescribable,” Lieberman said. “It gave me hope that we can alleviate the fear and anxiety associated with seizures. It would be life-changing for patients – both humans and animals – and their families.”
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see profile for Dr. Theodore Schwartz.
Syl Kacapyr is associate director of marketing and communications for Cornell Engineering.