Research led by Pennsylvania State University suggests that heparan-sulfate-modified proteins or proteoglycans (HSPGs) could be an effective early-stage target for new Alzheimer’s disease therapies.
Alzheimer’s disease is an ever-increasing neurodegenerative disease impacting up to seven million people in the U.S., most of whom are over the age of 65 years.
Developing treatments for this complex condition has proved difficult, with many failed, late-stage trials, but in the last couple of years there have been some successes. For example, the approval of the monoclonal antibody lecanemab in the summer of 2023, developed by Biogen and Eisai, to treat early-stage, symptomatic disease was the first really significant therapy approval for many years and provides proof of the so called “amyloid hypothesis” of the disease.
Similarly, another antibody treatment, donanemab, which was developed by Eli Lilly, has been approved by the FDA only this week, also for treating early-stage, symptomatic Alzheimer’s disease.
“Despite these successes, there is good reason to identify cellular and molecular pathologies that occur early in the Alzheimer’s disease process,” write Scott Selleck, a professor in the department of biochemistry and molecular biology at Penn State University, and colleagues in the journal iScience.
“Further investment in broad, mechanistic approaches to Alzheimer’s disease development is required to effectively prevent and treat this disease at a level that significantly alters the disease trajectory.”
In this study, Selleck and team assessed the function of HSPGs in Alzheimer’s disease by studying human and mouse cell lines, also using Drosophila as a model to assess the impact of HSPG changes on the drosophila version of the presenilin gene and mice to assess the impact of these proteins on APOE variants.
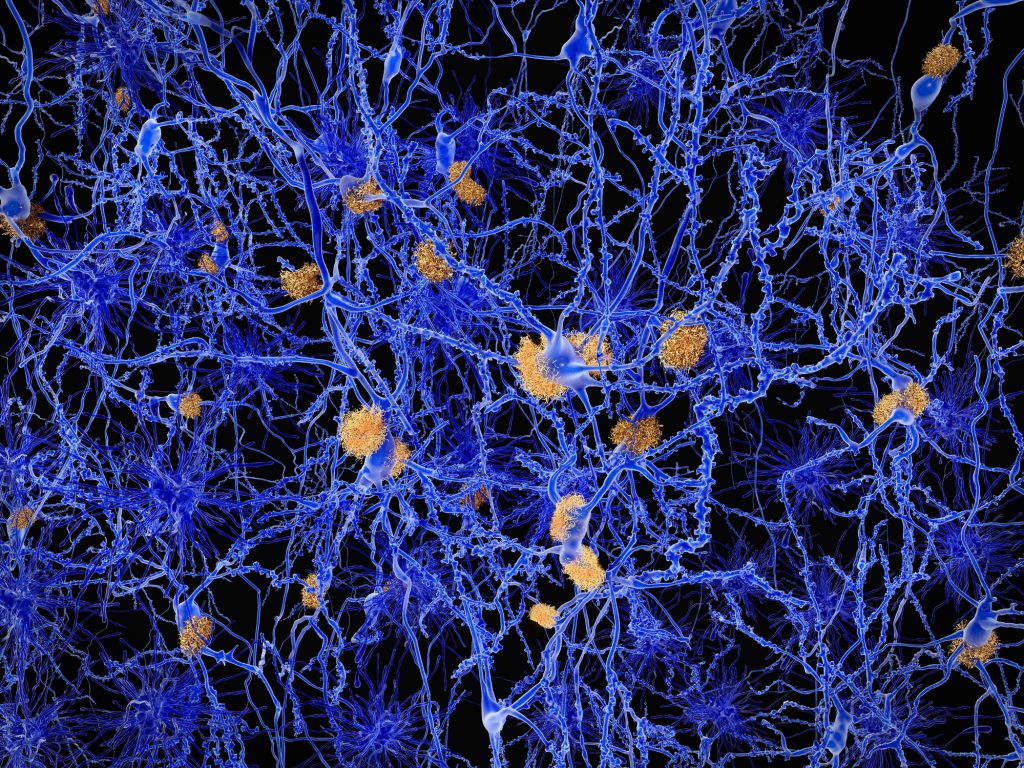
Mutations in the human version of the presenilin gene can cause Alzheimer’s disease. Normally, amyloid beta protein is formed when amyloid precursor protein is cut up by beta and gamma secretase enzymes. Presenilin forms part of gamma secretase and when it contains mutations, it cuts the precursor protein in a way that is more likely to form amyloid plaques. Similarly, people with some forms of the APOE protein, such as APOE4, have dramatically increased risk for developing Alzheimer’s.
HSPGs are found on the surface of cells and between cells. They attach to other proteins and by doing so form signaling pathways with several functions including directing how cells interact with the environment and regulating autophagy, a cell repair function that allows the clearing of dysfunctional or damaged parts of cells.
“In the early stages of several neurodegenerative diseases, autophagy is compromised, which means cells have a reduced repair capacity,” Selleck said in a press statement. This can allow things such as amyloid plaques to build up unimpeded.
The researchers found that changing the function of the HSPGs so they are less active can help restore autophagy and improve other physiological factors that can contribute to the very early stages of neurodegenerative disease such as lowering lipid build up and improving mitochondrial function.
“In this study, we determined that heparan sulfate-modified proteins suppress autophagy-dependent cell repair. What’s more, we show that by compromising the structure and function of the sugar modifications of these proteins, the levels of autophagy increase so cells can take care of damage,” noted Selleck.
In the animal and fly models of genetic Alzheimer’s disease, the researchers confirmed links between HSPGs and progression of the disease. When the researchers introduced a mutation into the human cell line that made it unable to make heparin sulphate, expression levels of over 50% of the genes known to be linked to Alzheimer’s disease were impacted.
“There is a critical need to focus on cellular changes that occur at the earliest times in disease progression and [to] develop treatments that block or reverse them,” Selleck said. “We demonstrate that reduced autophagy, mitochondrial defects and lipid build-up—all common changes in neurodegenerative disease—can be blocked by altering one class of proteins, those with heparan sulfate modifications. We think these molecules are promising targets for drug development.”